Healthcare still leads U.S. job growth; employers leaning into 'niche' benefits
Plus: A case study on how virtual medicine can help staff-starved rural hospitals
The healthcare sector added 72,000 new jobs last month, outpacing the monthly average of 60K new jobs over the past 12 months.
Healthcare led all sectors for job growth in March, according to government data, and accounted for 24% of all U.S. jobs created last month.
Leading the healthcare numbers were ambulatory care and hospitals with 28,000 and 27,000 new jobs, respectively; nursing and residential care saw more than 17,000 jobs created.
Employers are leaning into better benefits
A new report from Adzuna covered by Healthcare Dive finds that employers are investing in more perks and benefits to further improve recruitment and retention efforts, even as other industries have been scaling back on things like signing bonuses, expanded parental leave, and other competitive benefits.
“Healthcare and nursing employers are offering perks ranging from signing bonuses to fertility benefits in an attempt to lure workers onto payroll, according to an analysis from job search engine Adzuna,” Healthcare Dive wrote. “Tuition reimbursement, signing bonuses, and expanded maternity and paternity leave were the most common perks offered in healthcare job ads posted in February.”
Adzuna noted that niche perks tailored to specific workforce segments are growing more common as well.
“In particular, companies have been placing a heavier focus on female-centric perks like fertility benefits and menopause support in recent years,” said James Neave, head of data science at Adzuna, according to Healthcare Dive.
HCA Healthcare and Mayo Clinic were listed as examples of health systems investing in employee benefits packages, even as they’re cutting costs elsewhere.
California lawmakers consider letting community colleges offer nursing bachelor’s degrees
With California facing some of the nation’s most severe staffing shortages in nursing, the legislature is considering bills that would allow community colleges in the state to offer bachelor’s degrees in nursing, according to a new report by EdSource.
The proposal would allow 15 community college districts that already provide associate degrees in nursing to offer bachelor’s degrees in the field. Just over half of California’s bachelor’s and advanced nursing degree programs are at independent and private colleges, which hold about 51% of the market, EdSource said.
Statewide, there are 48 bachelor’s degree nursing programs; enrollment in bachelor’s nursing programs has increased statewide in recent years, and much of that growth has occurred at private institutions. Meanwhile, the report explained, fewer students are enrolling in associate degree nursing programs, which are mostly at public community colleges.
Estimates show California needs about 36,000 more licensed nurses than it has in the workforce, and the shortfall is expected to grow substantially by 2030, EdSource reported.
Read the full report here.
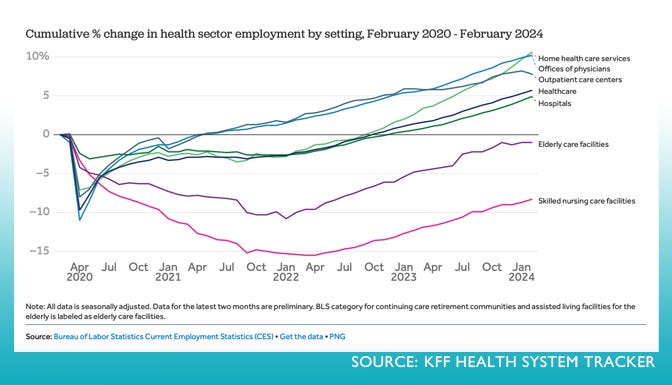
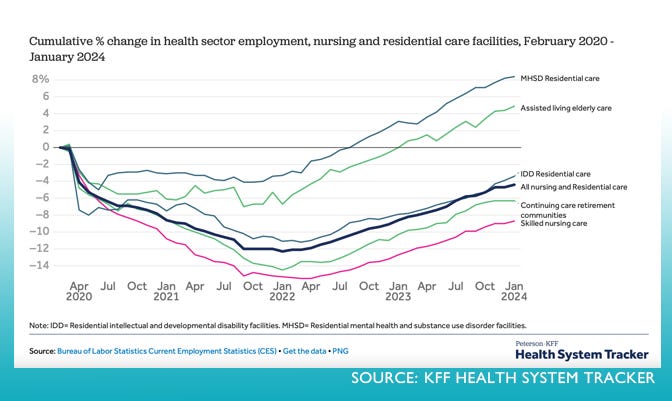
Updated charts tell the story of healthcare employment pandemic recovery
An updated collection of charts delves into employment data to analyze how jobs and wages in the health sector have changed since the COVID-19 pandemic. Unlike past recessions, health sector employment saw a big drop in early 2020 but has rebounded since, KFF Health System reports.
The charts are from the Peterson-KFF Health System Tracker, an online information hub dedicated to monitoring and assessing the performance of the U.S. health system.
A few examples that offer insights into recent employment trends in the industry:
Case study for understaffed rural hospitals: Virtual ICU
Rush Memorial Hospital in rural Indiana does not have the staff or resources for an ICU, which was a problem before the pandemic and moved to the top of hospital leaders’ priority list with COVID-19, according to a new report by Healthcare IT News.
“This was something staff was looking into even before COVID, as they were thinking about what was best for their patients and their families when it comes to being admitted to the hospital,” the outlet reported. “In addition, surgery staff was top of mind – without having an ICU, surgeons were less likely to perform certain surgeries. When COVID came and staff was faced with the inability to transfer, they knew it was time to do something different.”
With just two hospitalists on staff, the hospital knew they’d be inviting burnout if they expected them to perform intensive critical care 24/7, so Rush Memorial brought in vendor Access TeleCare to implement a two-bed, virtual ICU.
"We wanted to be able to open our ICU and have available the intensivist/ pulmonologist coverage our patients needed," Rush Memorial Vice President of Nursing Carrie Tressler told Healthcare IT News. "The added support would enable our hospitalists to focus on caring for higher-acuity patients, without having to transfer them to another facility."
The service enables the virtual providers to interact with patients via a HITRUST-certified telemedicine cart, each of which has full zoom-tilt cameras and integrated stethoscopes, so the virtual providers are able to get all the inputs they need to care for the patient adequately, the outlet reported.
How Rush Memorial’s virtual ICU works:
The virtual ICU providers are available overnight and handle admissions during those hours, transitioning the new patients to Rush Memorial hospitalists in the mornings.
The virtual ICU providers work closely with Rush’s emergency physicians and anesthesiologists for hands-on procedures to ensure continuity of care as patients are transitioned to the virtual providers’ care.
Access TeleCare's providers also work closely with Rush Memorial nursing staff on education and training on how to operate the ICU and are easily accessible to answer questions and provide guidance.
The virtual physicians have access to the electronic health records system used by the hospital, as well.
The results:
Hospital leaders report an increase in surgeries, Healthcare IT News wrote. “The virtual ICU has enabled surgeons to feel comfortable performing more surgeries, knowing they had available to them the clinical expertise to care for those patients in recovery in the ICU.”
Patient transfers to bigger facilities have decreased.
Patient experience feedback has improved, with even the older population “overwhelmingly” happy with the virtual care they’ve received.
Having on-site nurses involved in the virtual visits as well as the hospitalists checking on patients during their daytime rounds “has been helpful to the patient experience as it keeps a human element involved,” Tressler told Healthcare IT News.
Find the full report here.
Shout-out to Healthcare Workforce Report sponsors
The Healthcare Workforce Report newsletter is generously supported by MedCerts.
For information on supporting HWR, email HealthcareWorkforce@substack.com.