New Labor projections; who gets to be a ‘doctor’; and travel nurse pay comes down to earth – kinda
Also: A couple of articles offer a glimpse at how America's widespread 'healthcare deserts' are leading to actual deaths
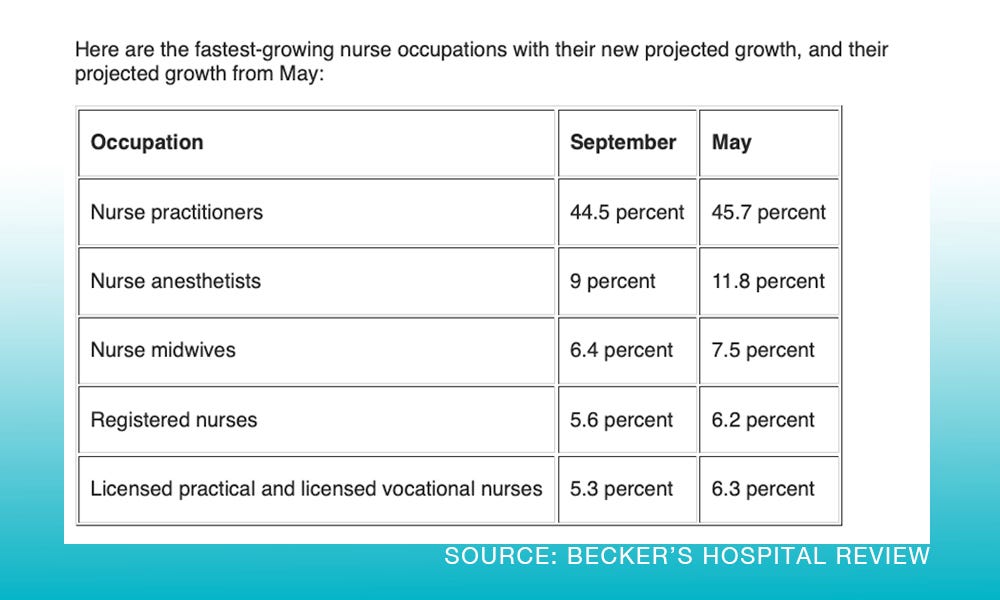
Within days of releasing its August jobs report (Surprise – healthcare gained a ton of jobs!), the Bureau of Labor Statistics updated its occupation projections for all jobs — and among the changes were some notable ones in healthcare.
All nursing jobs are projected to grow, but the BLS said it expected slightly less growth than previous data showed.
Nurse practitioner still has the highest projected growth through 2032 but it’s been adjusted downward — barely.
Physician specialties also saw some adjustments: The number of psychiatrists needed is predicted to grow the most, pediatricians the least. Read the details at Becker’s.
Healthcare job growth still leading monthly data! Who knew?
We all knew.
Still, the BLS data is helpful to the workforce planners, among others, so here it is.
Healthcare gained 70,900 jobs in August, according to the Bureau of Labor Statistics.
The August total is the biggest monthly gain for healthcare all year. And it’s 37% of ALL new jobs reported in the country last month.
The August data reveals that ambulatory healthcare services gained the most jobs at 39,900. Hospitals added jobs at a slightly slower pace in August, continuing a trend from the last several months.
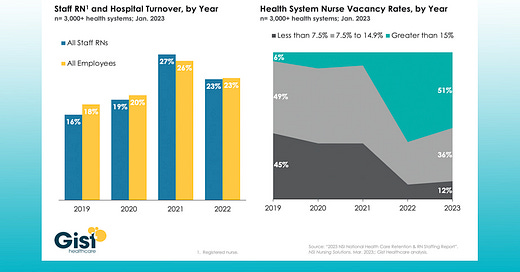
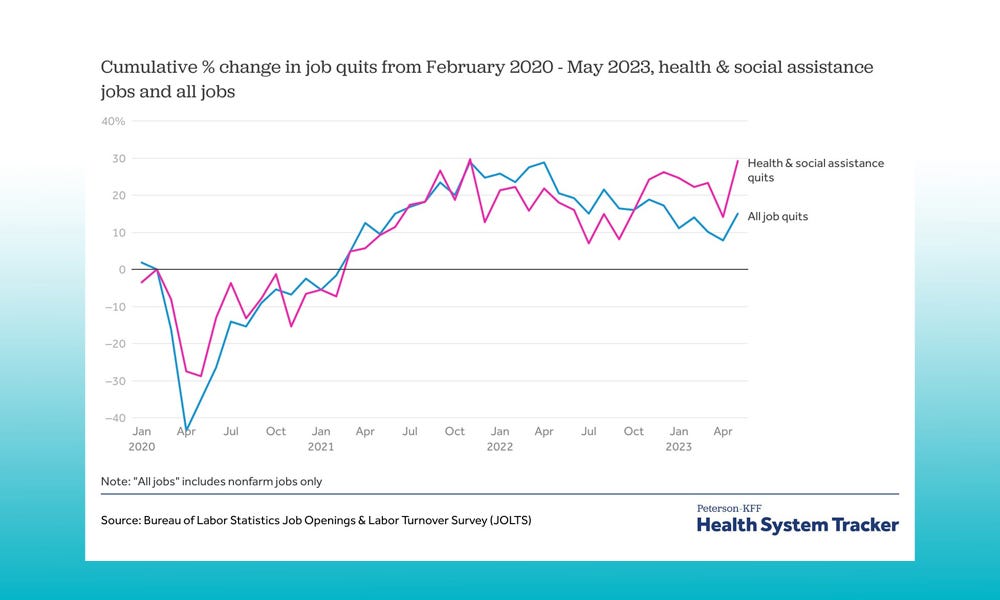
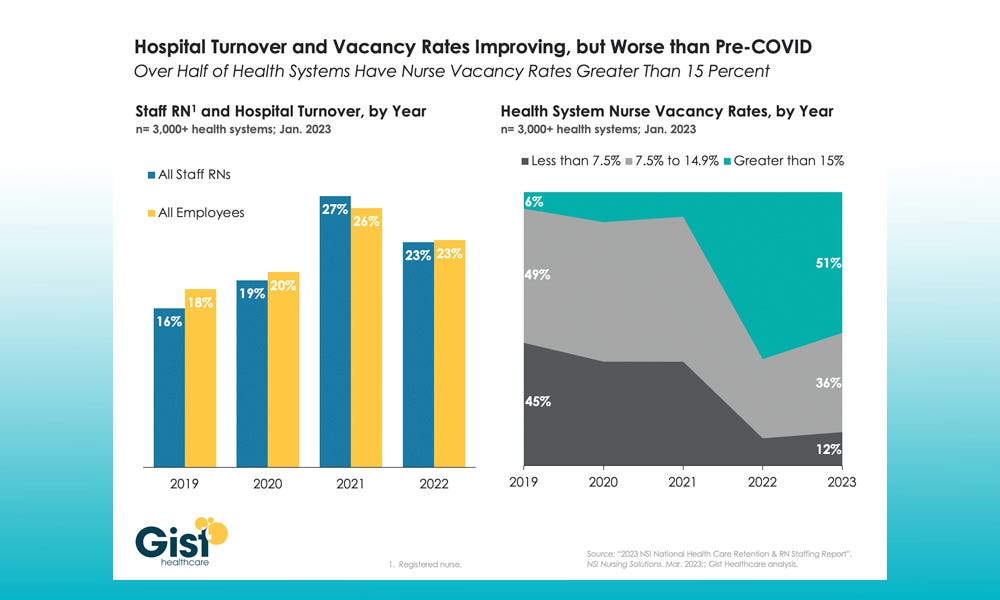
Two graphics: Healthcare workers still quitting in droves and hospital turnover is dropping – a little
Legal fight over who gets to use the title ‘doctor’
Interesting issue before a court in California currently, covered by Becker’s:
“The long-standing debate on non-physicians using the term ‘doctor’ is being highlighted in California after two advocacy organizations filed a court document in connection with a current case where nurse practitioners want to be referred to as doctors.”
Three nurse practitioners with doctorates are suing so they can use the terms, but California has a long-standing law that prohibits use of the title "doctor" or "Dr." by anyone other than qualified physicians.
The debate has taken on more currency recently, according to recent Becker's coverage, as physician shortages continue, with 27 states now allowing nurse practitioners to practice without physician supervision. And with shortages not likely to ease soon, the issue of titles is the surface of a much deeper issue that a lot of states have yet to address: who can be a primary care provider, if the “traditional” primary care providers are vastly unavailable in so-called healthcare deserts?
I’d love to hear your thoughts on this, by the way. Email me or comment!
Speaking of healthcare deserts: 80% of us live in them
In a recent op-ed in the Arkansas Democrat-Gazette, author Chris Jones, Ph.D., calls attention to some new stats about how the shortage of healthcare workers is impacting real-life across the United States and particularly in Arkansas.
Excerpt:
In a nation known for its technological advancements and economic prowess, the stark reality is that more than 80 percent of Americans live in healthcare deserts. Nowhere is this concern more pressing than in Arkansas, where 41 percent of our citizens reside in rural areas lacking essential healthcare services.
The Center for Healthcare Quality and Payment Reform has issued a sobering statistic: More than 600 rural hospitals nationwide are in jeopardy of shutting down within the next year. In Arkansas, this includes a staggering 23 of 53 rural hospitals.
The situation has turned critical. An investigation by the Arkansas Advocate revealed that every county in our state is grappling with an ambulance shortage, meaning paramedics must drive 25 or more minutes to reach someone in need of life-saving care.
Our neighbors in rural communities face a higher risk of premature death from heart disease, cancer, chronic lower respiratory disease, and stroke. Unintentional injuries cause up to 50 percent more deaths in these areas compared to cities.
Jones’ article (and the Arkansas Advocate report) include a lot more alarming information about how healthcare workforce shortages are leading to actual avoidable deaths in rural communities and particularly in Arkansas.
PS: This is why I care about healthcare workforce topics and why you should, too. Subscribe now (it’s free, thanks to our sponsor MedCerts!) and support this work with your eyeballs. Thanks in advance.
Travel nurse pay comes back down to earth – kinda
A recent Emergency Medicine Workforce Newsletter (which by the way I highly recommend – a great read every week!) discussed a recent survey of travel nurses, a field that exploded in popularity and in pay during COVID.
Travel nurses were “raking in up $10,000 a week during the pandemic’s peak, that dropped to an average of about $3,000 this year,” EM Workforce reports.
According to Vivian Health, a national health care hiring agency, the average weekly pay for U.S. travel nurse pay in December 2022 was $3,177, down 16% from December 2021′s $3,782.
“Good money isn’t the only reason travel nurses don’t stay in one place, however, according to the survey. Almost as important was freedom and flexibility, with 67% listing it as a motivator. According to the survey, 41% said they would never go back to a staff position.”
Read the rest at https://emworkforce.substack.com.
Shout-out to Healthcare Workforce Report sponsors
The Healthcare Workforce Report newsletter is generously supported by MedCerts.
For information on supporting HWR, email HealthcareWorkforce@substack.com.