Osteopathic medical education is expanding (and why that matters for primary care shortages)
Plus: Cleveland Clinic heads to the Heartland and how the Physician Assistant role is changing
First, the latest jobs report:
Like the U.S. economy as a whole last month, healthcare saw better-than-expected job growth, with the sector adding 45,000 new jobs — about 30% more than the month before. Still, September’s total was lower than the average monthly growth over the previous 12 months, according to the Bureau of Labor Statistics.
It was the third consecutive month in which healthcare job growth slowed slightly but remained robust, Health Leaders Media noted. Healthcare jobs accounted for nearly one-fifth of all new jobs reported last month; home healthcare services added the most with 13,000, and hospitals followed with 12,000 new jobs, HLM reported.
Growing DOs: Colorado breaks ground on osteopathic medical school
Osteopathic medical education is expanding.
University of Northern Colorado recently held a groundbreaking celebration for its planned College of Osteopathic Medicine, which will be the state’s third medical school. State funding was approved earlier this year as access to primary care worsens across much of Colorado.
The college expects to open in the fall of 2026; it will graduate 150 new doctors each year, state officials have said. According to the federal Health Resources and Services Administration, just 34.6% of Colorado’s needs for physicians is met, and 59 of Colorado’s 63 counties contain Health Professional Shortage Areas in primary care.
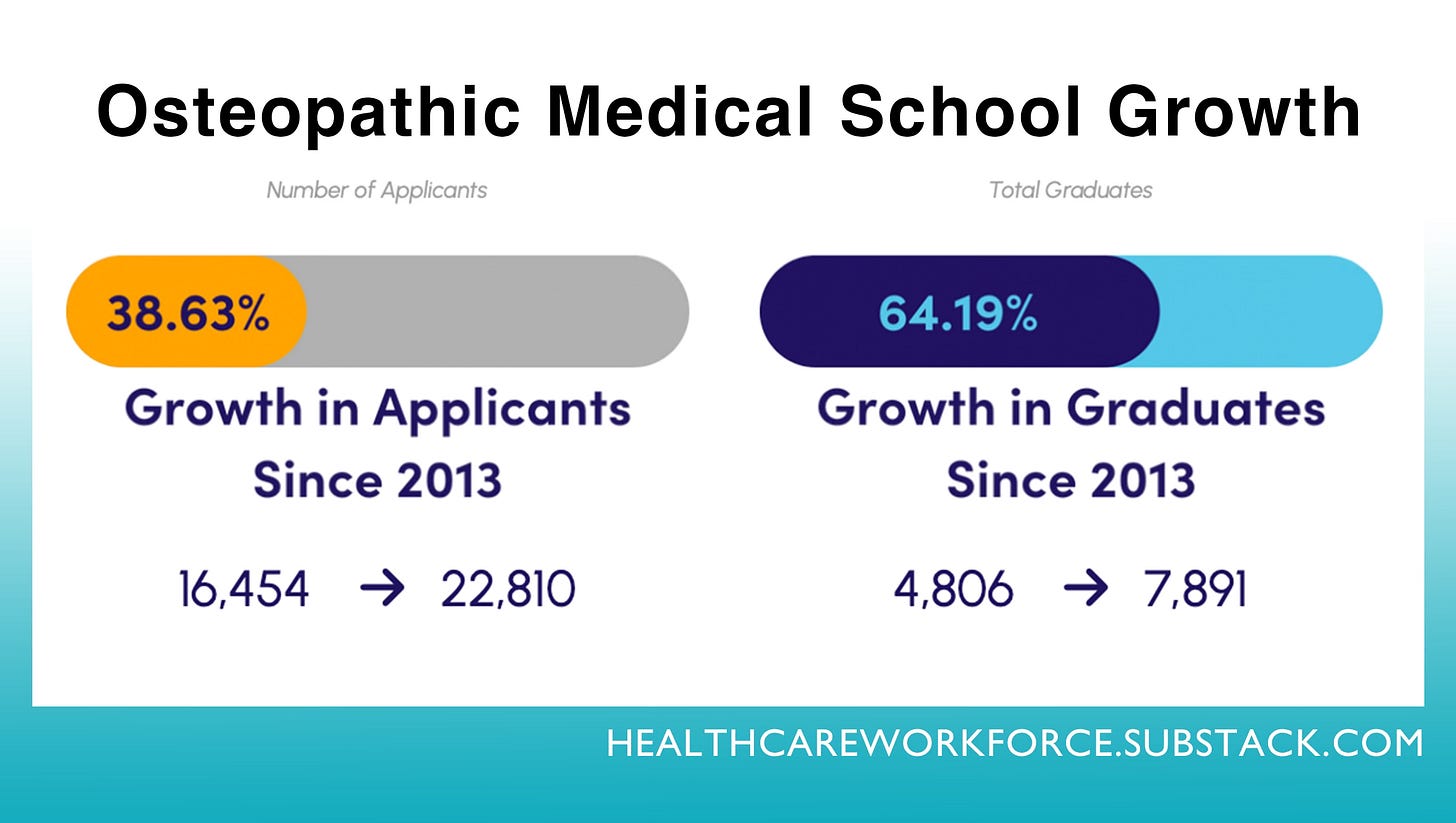
Nationally, osteopathic medicine has been having a moment, so to speak, in recent years: Last academic year, 38,000 students were studying to become osteopathic physicians, which is a record high and a 65% increase since 2013, according to the American Association of Colleges of Osteopathic Medicine.
Colorado’s new osteopathic college will be the 43rd accredited osteopathic medical school in the country, and several more are in the works, AACOM says.
Osteopathic medical schools typically turn out a far higher percentage of primary care physicians versus MD programs: 57% of DOs practice in primary care, while only 28% of MDs in the United States are primary care providers, according to the American Medical Association website.
As a result of the growth in the DO field, healthcare access advocacy groups like AACOM are lobbying Congress to pass several DO-related bills such as expanding residency opportunities and community-based education programs in underserved areas.
Cleveland Clinic heading into the ‘heartland’ and a ‘holistic’ healthcare push
The Alice L. Walton Foundation recently unveiled a $700 million, 30-year partnership with Mercy, Heartland Whole Health Institute, and Cleveland Clinic to radically expand access to specialty healthcare and improve health outcomes in the “heartland,” which in this instance means Northwest Arkansas and the surrounding region that the Rogers, Arkansas market serves: southwest Missouri, southeast Kansas, and northeast Oklahoma.
Northwest Arkansas is the 18th fastest-growing MSA in the country and is home to the headquarters of Walmart, Tyson Foods, J.B. Hunt Transport, and Arvest Bank — as well as offices of every company whose products are sold in Walmart stores. Alice Walton is the daughter and an heir of Walmart’s founder, Sam Walton.
Her own healthcare difficulties led to Walton’s launch in 2019 of the Heartland Whole Health Institute, which aims to “transform health care by improving outcomes, reducing costs, and expanding access, beginning in the Heartland and scaling nationally,” according to the institute’s website.
“Its purpose is to lower costs, improve quality, and broaden access to healthcare in the Heartland by catalyzing new delivery models, using whole health principles, that can be replicated to disrupt the national health care system.”
FWIW: This stated “purpose” likely sounds incredulous to anyone unfamiliar with the Waltons and their philanthropic track record. But if anyone can do it, Alice Walton can. (See also: Crystal Bridges Museum of American Art, another massive philanthropic project solely funded by Alice Walton that silenced even the most skeptical critics when it opened in 2011.)
Just one year into planning her Heartland Whole Health Institute, Walton’s foundation announced it would fund a new medical school as well, named the Alice L. Walton School of Medicine. It is set to open for students next fall.
The new affiliate partnership with Cleveland Clinic follows several years of planning, jump-started by a 2020 study that showed many leave the region for specialty care and in particular for cardiology services.
Mercy and the foundation are each investing $350 million, according to the news release, to develop a cardiac care center and a virtual care center, for starters. The cardiovascular center will be co-branded by Mercy and Cleveland Clinic.
Also within the announcement is the news that Mercy will serve as the primary educational partner for Walton’s new medical school. Mercy said it anticipates these developments will lead to “hundreds” more physicians practicing in Northwest Arkansas within the next five to seven years.
Five ways PA roles are changing
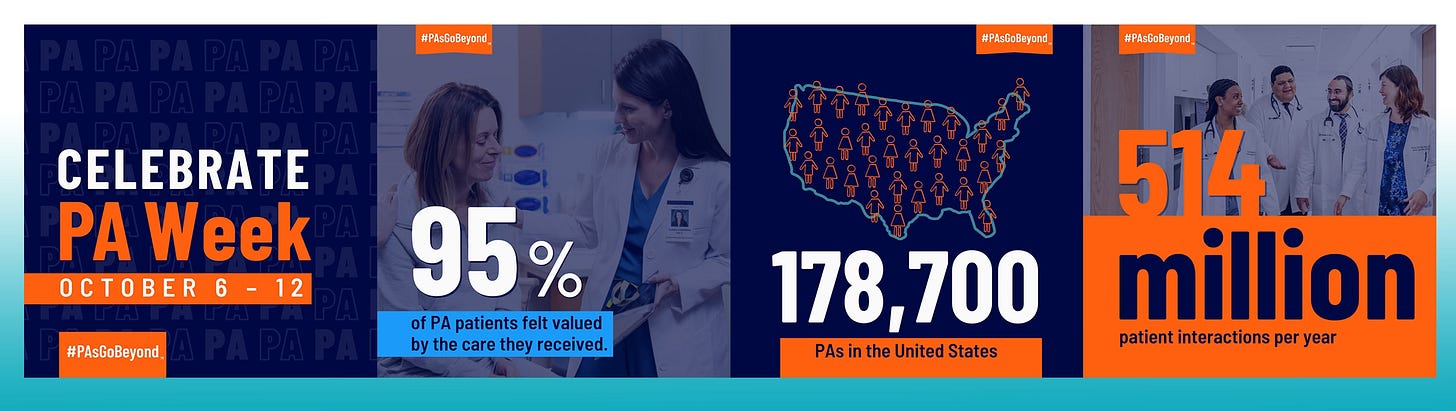
This week is Physician Assistant Week, calling attention to the 178,000 PAs practicing in the United States and how they improve care for patients across all practice areas.
PA roles are transforming, according to a new report from University of Arizona Health Sciences (UAHS), in part because PAs are increasingly stepping up to serve as primary care providers for the 78 million Americans living in areas with physician shortages.
The job of Physician Assistant — ranked No. 2 in Best Health Care Jobs by U.S. News & World Report — is seeing “five emerging trends,” according to UAHS.
Expanding scope of practice: Some states are updating laws to allow PAs to establish their own practice without requiring a supervising physician to oversee clinical care; Arizona just did this for PAs with 8,000 hours or more of clinical experience.
Embracing leadership roles: Around 94% of healthcare organizations offer structured leadership pathways for PAs, and “PAs are taking on essential roles that influence health care delivery at a systemic level,” UAHS says.
Virtual medicine and technology-driven care: PAs are “at the forefront” of healthcare’s digital transformation and are specifically trained to use telehealth in managing patients’ chronic conditions such as diabetes and hypertension remotely, according to UAHS.
Advanced education and specialized training: Advanced education for PAs is expanding, with a growing number pursuing doctorate degrees and specialized residencies. The National Commission on Certification of Physician Assistants now offers board certification in 11 medical and surgical specialties, with more in development.
Growing salary and job opportunities: As physician shortages continue to fall short of demand, PA job openings are rising, as are average salaries. The median salary in Arizona is around $127,000, up about 3.5% from last year, according to UAHS.
Shout-out to HWR sponsors
The Healthcare Workforce Report newsletter is generously supported by MedCerts.
For information on supporting HWR, email HealthcareWorkforce@substack.com.