Report: Increasing salaries, benefits as a tool in a tight labor market is losing impact
Compensation has risen 40% since 2019 for some roles; more room to grow deemed unlikely with profit margins under pressure
Confession: I’m secretly a math and data nerd, and this week’s issue will deep-dive into one of the most comprehensive and important industry-specific research reports I’ve seen in a hot minute. The data is pretty interesting for any healthcare employer, healthcare worker (any level), or would-be healthcare worker.
The report, 2024 MGMA Management and Staff Compensation Report, released a few weeks ago, even includes some data on how many organizations are turning to AI tools to boost efficiencies in some departments, such as revenue cycle management.
The report can be downloaded directly from MGMA, and it’s worth the effort. Its data is based on surveys of more than 171,000 healthcare workers, hiring managers, executives, and frontline staff positions including clerical staff. The surveys were conducted between October 2023 and May 2024. HealthcareDive.com also offers a good breakdown, some of which is quoted here.
Let’s dig in.
Context: Given the labor shortages pressuring healthcare organizations and the projections that they will get worse before they get better, employers have relied largely on raising wages and beefing up their benefit packages to better compete for qualified workers, from receptionists to medical assistants and from patient care assistants to nurse practitioners and medical doctors. Sign-on bonuses for nurses and doctors have expanded by thousands — though some industry voices encourage investing those dollars in training new members of the labor pool instead.
Key findings about compensation growth:
In 2023, compared to the year before:
Median total compensation grew:
3.3% or about $0.57 per hour for medical assistant positions
$1.61 per hour more for certified nursing assistants
$2.15 per hour more for patient care assistants
$1.65 per hour more for RNs
$1.19 per hour more for licensed practical nurses
Median total compensation for healthcare management positions grew 7%.
Some employers also offered enhanced benefits, such as reimbursement and paid time off for education, new wellness benefits, better mental health resources and paid leave.
Despite investing more in pay and benefits, 80% of employers said they spent more time trying to hire in 2023 than in previous years.
This year so far, compared to 2023:
70% of respondents told the MGMA that their benefits packages stayed largely the same.
9% said their benefits offerings had declined in 2024.
“Increasing compensation cannot fully address labor shortages, according to the MGMA,” Healthcare Dive wrote. “The most successful medical groups are employing a broad range of strategies to optimize their workforce, including building new graduate programs and leveraging artificial intelligence.”
Employers’ reluctance to increase benefits and perks could also be due to a lack of return on investment, according to the report.
The MGMA report noted that some of the lingering staffing shortage in 2024 is due to structural “bottlenecks” across the healthcare labor market that are unlikely to be solved through increased compensation alone.
“For example, since the pandemic, new nurses have been hard to come by as budget cuts and a lack of faculty have forced baccalaureate nursing programs to turn away record levels of qualified candidates, according to the American Association of Colleges of Nursing, which tracks enrollment trends over time.”
AACN says that 55,111 qualified applicants were turned away from entry-level baccalaureate nursing programs in 2023, a slightly less dire total than the 66K in 2022 and the 76K turned away in 2022.
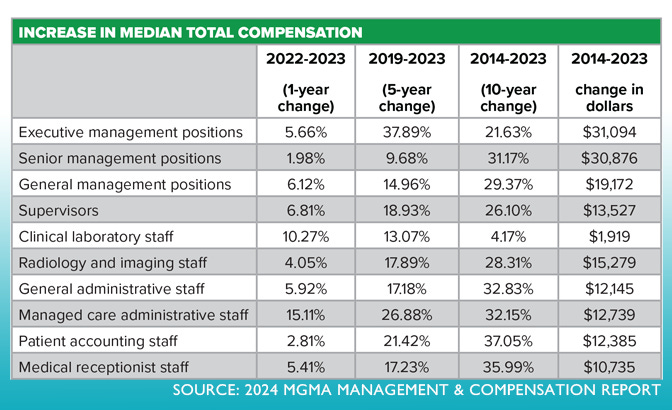
Compensation changes over the past 5 years (2019 through 2023):
Registered nurse median compensation has increased by 19.6%.
Medical assistant compensation surged by 20.6%.
Licensed practical nurse compensation rose by over 22%.
Compared to pre-pandemic (2019) benchmarks, total median compensation through 2023 has grown:
26.88% for managed care administrative staff
21.42% for medical receptionist staff
17.89% for radiology and imaging staff
17.23% for medical receptionist staff
17.18% for general administrative staff
What’s working well for some employers in a difficult labor market:
Among the respondents who reported improved recruiting efforts, the common factors they shared about their successes included:
Building or investing in new graduate programs and/or residencies for RNs to address nearby nursing school capacity limits and prioritizing hiring newly graduated nurses
Investing in upskilling current staff into new roles
Increasing compensation and benefits to compete more effectively with larger organizations
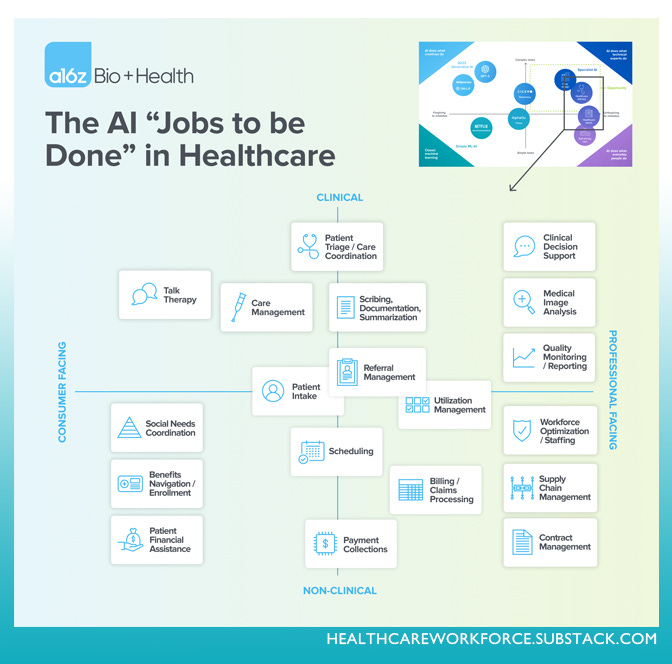
Almost 50% of medical groups surveyed in February 2024 had begun to automate their revenue cycle operations, and 17% had automated more than 60% of revenue cycle operations
Leveraging AI to do more with less staff
Speaking of AI in healthcare …
“The hot topics of using AI in healthcare, confronting physician burnout and easing EHR burdens in medical groups often converge on a single topic: using scribes, human or machine,” MGMA said in the report.
A Dec. 5, 2023, MGMA Stat poll found that in the past year, about 25% medical group leaders added or improved their use of scribes — human or machine — in their organizations. The poll had 415 applicable responses. In 2023 MGMA polls, 74% of medical groups had not added or expanded use of AI tools.
Why all of this matters
About half of medical groups report their visit volumes in 2024 are above levels seen at the same time last year — more evidence of a surge in demand for healthcare, which, coupled with workforce shortages, is usually bad news for patients and health outcomes, reflected in the new MGMA data as well:
38% of medical groups reported patients’ time to appointment/access grew longer in 2023 over the year before
38% said it was unchanged
24% reported improvements
Another recent survey of just doctors, reported in the June 20, 2024, edition of this newsletter, shows 82% of physicians said their organizations’ staffing shortages have negatively impacted patients:
87% said longer wait times
75% said diminished access to care
75% said worse healthcare disparities
74% said frustration or anger
70% said delayed treatment
42% said worse or preventable outcomes
36% said later-stage diagnosis
Shout-out to HWR sponsors
The Healthcare Workforce Report newsletter is generously supported by MedCerts.
For information on supporting HWR, email HealthcareWorkforce@substack.com.